CASE STUDY
Using data to reconstruct missing bone for revision surgery
Revision hip surgery often presents a major challenge: parts of the acetabulum may be missing or severely damaged due to disease, loosening, infection, or multiple previous operations. Without reliable anatomical landmarks, planning the placement of a new implant becomes extremely complex.
Our team uses statistical shape modelling (SSM) to solve this problem. By analysing patterns of pelvic shape across large datasets, we can estimate where missing bone would have been before the defect occurred. The model generates a personalised reconstruction of the patient’s likely anatomy, providing a more accurate reference for planning.
This approach helps surgeons:
• Identify the ideal centre of rotation and socket orientation
• Design custom implants tailored to the true underlying anatomy
• Improve implant stability and restore more natural joint mechanics
By integrating imaging, computational modelling, and surgical expertise, we enable more precise planning in some of the most challenging revision cases; ultimately supporting better outcomes for patients.
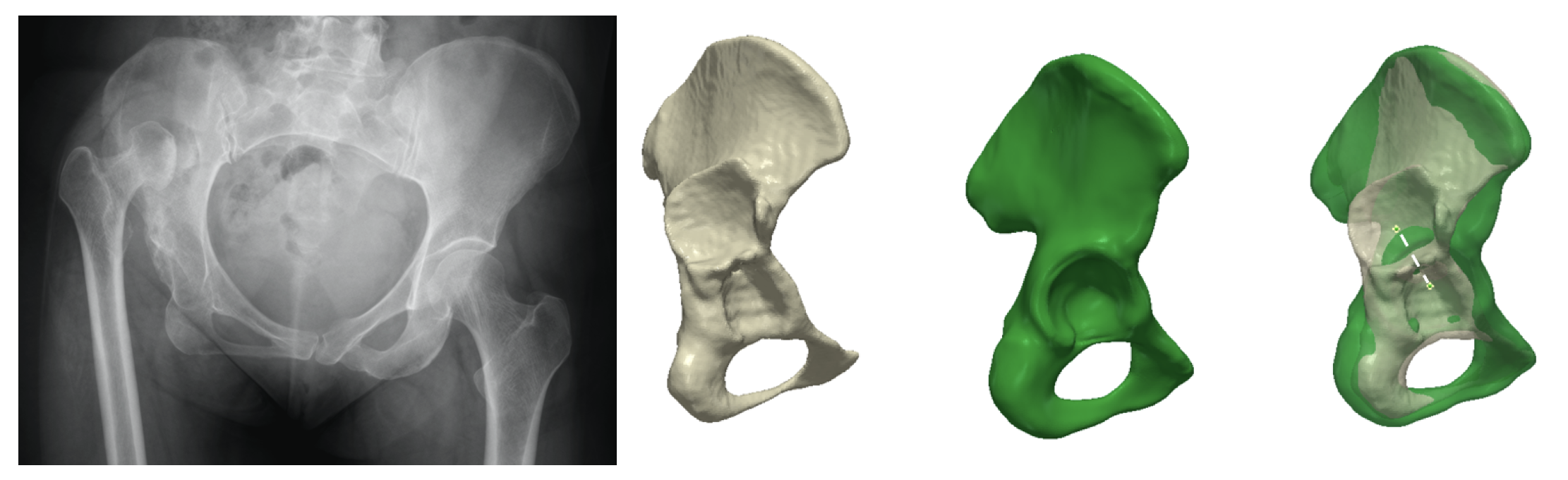
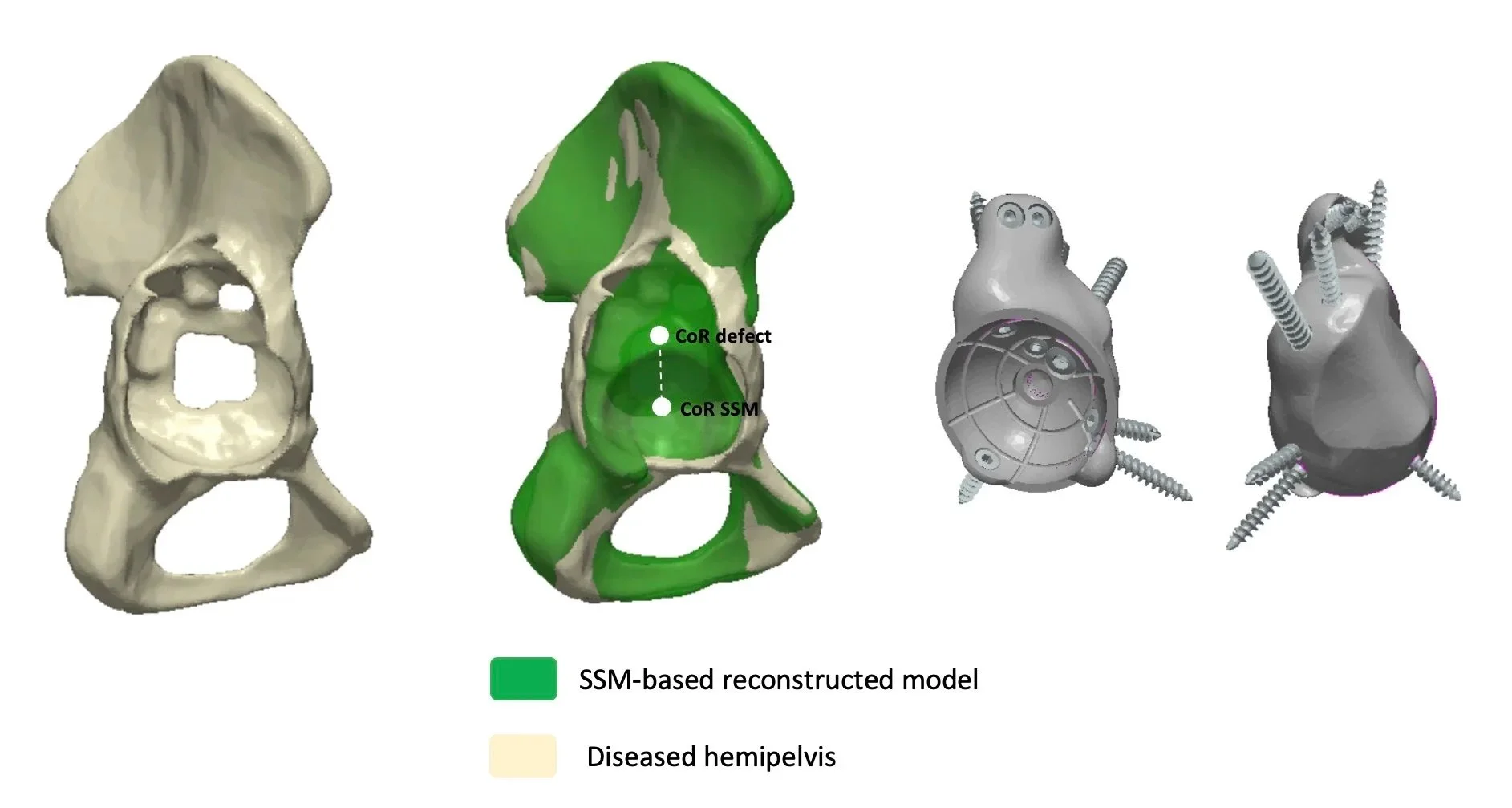
Left to right images. Anteroposterior plain radiograph shows developmental dysplasia of the right hip with a high hip centre. 3D reconstruction of a native dysplastic anatomy (white 3D model) ; SSM model-based reconstruction (green model); Overlap between the native anatomy and its SSM-based reconstruction showing the difference in Centre of Rotation.
The challenge
In revision hip surgeries, large parts of the socket (acetabulum) may be missing. This makes it difficult to know where to place the new implant.
Our solution: modelling bone landmarks
To address missing or distorted anatomy in revision surgery, we developed a data-driven method to reconstruct the bone landmarks normally used to guide implant positioning. Using statistical shape modelling, we analyse healthy acetabular anatomy across large datasets and fit this model to the patient’s remaining bone to estimate where key landmarks, such as the acetabular rim and centre of rotation, would have been before the defect occurred.
This approach “fills in the gaps,” giving surgeons a far more reliable anatomical map than imaging alone in cases of severe bone loss. The reconstructed landmarks support the design of custom 3D-printed implants, helping determine optimal positioning, improve load transfer, and restore natural joint biomechanics. In challenging revision cases, this technique offers a powerful way to plan reconstruction with greater accuracy and confidence.
Why it matters
This technique helps surgeons better plan revision procedures and improves the fit and stability of implants in difficult cases.